Bacterial pathogens, antimicrobial resistance, and antibiotics
Antimicrobial resistance, or the ability of microorganisms to resist the drugs designed to inhibit or destroy them, is a critical, emerging threat with global ramifications. In 2021, antimicrobial resistance was linked to 4.71 million deaths, with 1.14 million directly attributable fatalities. Projections indicate that by 2050, these numbers could rise to 8.22 million and 1.9 million, respectively [1].
The largest percentage of antimicrobial resistance is caused by a group of highly resistant bacteria collectively called ESKAPE: Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter spp. These pathogens share some common characteristics and exhibit high resistance due to their genetic adaptations and mechanisms, including drug inactivation via enzyme production, activation of efflux pumps, outer membrane modifications, permeability changes, and the bypassing of metabolic pathways. Despite the introduction of new antibiotics like β-lactamase inhibitors and glycopeptides, which are design to treat bacteria such as Methicillin-resistant Staphylococcus aureus (MRSA) or Vancomycin-resistant Enterococcus faecium (VRE), resistance continues to evolve [2].
Combating these pathogens requires a clear understanding of the interactions between the antibiotic and its target, informing the development of novel chemical scaffolds with improved potency and efficacy. This process is a vital part of ongoing drug discovery, particularly in the rational, structure-based drug design (SBDD) of antibiotics. Cryogenic electron microscopy (cryo-EM) is a valuable structural biology technology that enables the visualization of these mechanisms at unprecedented detail, accelerating the development of novel antibiotics.
Drug discovery of allosteric gyrase inhibitors to treat fluoroquinolone-resistant bacteria
Multi-drug-resistant gram-negative bacteria, such as Escherichia coli and Klebsiella pneumoniae, have evolved resistances to a variety of third-generation cephalosporins, carbapenems, and fluoroquinolones, underlining the pressing need for new antibiotics. Using a phenotypic screening approach, researchers from Leiden University discovered of a novel class of isoquinoline sulfonamides, with LEI-800 in particular identified as a small molecule lead compound. LEI-800 exhibits outstanding potency against fluoroquinolone-resistant gram-negative bacteria along with low cytotoxicity in mammalian cells and no cross resistances with fluoroquinolones.
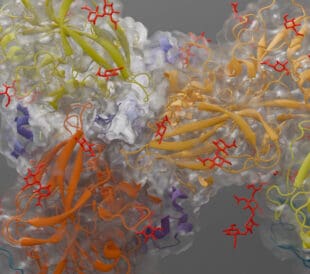
Cryo-EM revealed how LEI-800 binds to its target, the bacterial DNA gyrase, specifically showing that LEI-800 binds to an allosteric, hydrophobic pocket, distinct from the binding sites of fluoroquinolones and other known gyrase inhibitors. This novel binding mechanism prevents DNA cleavage, thus inhibiting bacterial replication, underlining the therapeutic potential of LEI-800 as a next-generation antibiotic that targets multi-drug-resistant gram-negative bacteria [3].

Mode of action of LEI-800 binding and inhibiting bacterial DNA gyrase. Figure reproduced from Bakker et al. under CC BY 4.0.
Novel classes of antibiotics target carbapenem-resistant Acinetobacter strains
Gram-negative bacteria are difficult to combat due to their complex outer membranes, which mainly consist of lipopolysaccharides (LPS) and make them resistant to most antibiotics. Several research groups at Roche identified a new class of macrocyclic-peptide antibiotics, which have been proposed to target and inhibit the LPS transport machinery [4]. These peptides display high potency and selectivity against Acinetobacter strains, including carbapenem-resistant A. baumannii.
High-resolution cryo-EM structures of these peptides in complex with the LPS transport machinery show binding of the peptides to a composite site formed by the transporter and its LPS substrate. This traps the transport system in an LPS-bound state and blocks LPS from reaching the outer membrane. The resulting toxic accumulation of LPS intermediates within the bacteria leads to cell death. High specificity for Acinetobacter was found to be a result of differences in the Lpt proteins and LPS-binding pockets across different gram-negative bacteria. These findings provide a foundation for the design of similar inhibitors for other gram-negative bacteria [5].

Composite binding pocket of macrocyclic peptides with LPS in complex with the Lpt transporter machinery. Figure reproduced from Pahil et al. under CC BY 4.0.
In the same year, researchers at Merck & Co. Inc. discovered a novel class of antibacterial compounds named cerastecins. These target the A. baumannii MsbA transporter, a key component of the lipo-oligosaccharide (LOS) transport pathway in the outer membrane of gram-negative bacteria. LOS biogenesis and transport are both essential for bacterial virulence and survival, making MsbA a promising target for antibacterial therapy.
Cerastecin A and B, potent inhibitors of MsbA, were found via high-throughput screening and display a narrow-spectrum of antibacterial activity. Cerastecin B in particular shows strong activity against clinical carbapenem-resistant A. baumannii isolates. The cryo-EM structure of cerastecin B-bound MsbA reveals a unique serpentine inhibitor configuration that stalls transporter activity and decouples ATP hydrolysis from LOS flipping. This disrupts LOS transport to the outer membrane and ultimately decreases the integrity of the bacterial membrane. Overall, cerastecins are exciting, potential narrow-spectrum antibiotics and their discovery paves the way for further rational design of derivatives for the treatment of other carbapenem-resistant Acinetobacter strains [6].

The unique serpentine configuration of cerastecin C in complex with MsbA. Figure reproduced with permission from Daniel J. Klein, Merck & Co. Inc.
Combating antimicrobial resistance via accelerated development of novel antibiotics
Microorganisms inherently evolve mechanisms to survive exposure to antibiotics, and antimicrobial resistance is ultimately caused by several factors including overuse and misuse of antibiotics, incomplete treatments, poor infection control, as well as global travel and trade. There is a pressing need for next-generation antibiotics that function despite these factors, effectively circumventing antimicrobial resistances to combat disease.
With SBDD approaches, researchers can optimize antibiotic precursors at the molecular level, enabling the development of lead compounds that display greater efficacies and less side effects. Cryo-EM accelerates this rational design approach with the visualization of molecular interactions at regular decision-making steps of the drug discovery process. We hope that novel lead compounds discovered with cryo-EM continue to pave the way to a future where antibiotics surpass the development of antimicrobial resistances.
References
[1] Global burden of bacterial antimicrobial resistance 1990–2021: a systematic analysis with forecasts to 2050 – The Lancet
[2] ESKAPE pathogens: antimicrobial resistance, epidemiology, clinical impact and therapeutics – Nature Reviews Microbiology
[3] Discovery of isoquinoline sulfonamides as allosteric gyrase inhibitors with activity against fluoroquinolone-resistant bacteria – Nature Chemistry
[4] A novel antibiotic class targeting the lipopolysaccharide transporter – Nature
[5] A new antibiotic traps lipopolysaccharide in its intermembrane transporter – Nature
[6] Cerastecins inhibit membrane lipooligosaccharide transport in drug-resistant Acinetobacter baumannii – Nature Microbiology


Leave a Reply